On Oct. 27, 2003, Michael
Schiavo, the husband of the cognitively disabled Florida woman, Terri
Schindler-Schiavo, appeared on Larry King Live to explain why he was fighting
so hard to remove his wife’s feeding tube.
His appearance
was only days after the Florida legislature intervened to have Terri’s
feeding tube reinserted for the second time in two years.
Michael Schiavo insisted that he wanted to help his wife
“die with dignity.” He told King: “It’s painless, and
probably the most natural way to die. It is a very easy way to die —
probably the second best way to die, the first being an aneurysm.”
At the same time
he was speaking on national television, Terri’s medical file contained
a document prescribing for her a slow and painful death by starvation and
dehydration.
Called an “Exit Protocol,” the document contains explicit instructions
for how Terri will be treated during the grisly series of events that will
occur should the courts decide to withdraw her feeding tube. Terri’s
fate remains an active issue in both the Florida state and U.S. federal
courts.
The nurse who discovered the Exit Protocol, Cheryl Ford,
R.N., a Tampa nurse, was reviewing Terri’s medical file at the request
of the Schindler family when she found the document. For the benefit of our
readers, Ford agreed to explain this document in detail. [Editor’s note:
The protocol, in bold print, is followed by Ford’s comments.]
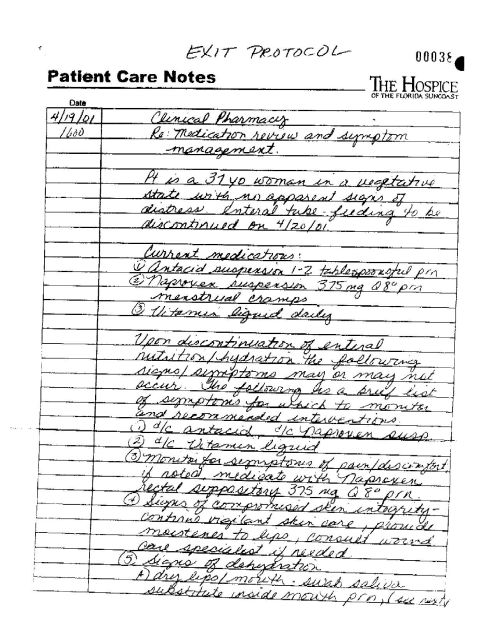
• Patient Care Notes—
The Hospice of Florida Suncoast — 4/19/01 — Clinical Pharmacy —
Re: Medication review and symptom management. The patient is a 37-year-old
woman in a vegetative state with no apparent signs of distress. Enteral
tube-feeding to be discontinued on 4/20/01.
“This is a very critical
piece of information from a nurse’s point of view,” Ford said.
“We have a patient with no apparent signs of distress, yet enteral tube
feeding is going to be discontinued on 4/20/01. This is murder. And it’s
premeditated murder, because look at the dates — notes were prepared
the day before the tube was supposed to be withdrawn.”
What would make the death more difficult is that Terri
is a healthy woman, weighing approximately 138.5 pounds, which means she
will endure longer than other patients who are in the midst of a natural-death
process.
“I was an oncology (cancer) nurse,” Ford said.
“These people are very weak and gaunt. Their bodies are already shutting
down, and their tube feedings are withdrawn when their body systems can no
longer handle it. But Terri is not a cancer patient — that’s what
bothers me. She’s a healthy young woman.”
• Upon discontinuation
of enteral feeding the following signs/symptoms may or may not occur. The
following is a brief list of symptoms for which to monitor and recommended
interventions.
• Monitor symptoms of pain/discomfort. If noted, medicate with Naproxen
rectal suppository 375 mg. Q8 prn [“Q8 prn” means eight times a
day as needed].
If someone in a persistent
vegetative state cannot feel pain, as Michael Schiavo and his attorney, George
Felos, have consistently told the world, why do Terri’s charts tell
nurses how to treat her for pain?
According to Ford, that is because Terri can and will feel pain during this
process — and a lot of it.
“Think about what hunger pains
are like if you haven’t eaten in a while,” Ford said. “You
start to get that gnawing feeling, almost a burning in your stomach. Most
people don’t extend themselves into the depths of hunger. They grab
a cracker or bread if they’re out shopping for a while just to make
themselves feel better.”
Terri would not have this option, however. “Within several hours,
she’ll start to feel this kind of hunger pain,” Ford said.
Dehydration would only add to the discomfort: “When
she starts going into the dehydration stage, her metabolism will start to
change. Her electrolytes will get imbalanced. She’s going to get
uncomfortable and will start to writhe.
“Advance a couple days without food or water. Now
her mouth is parched, her lips, her gums, her tongue will start to crack
and bleed. The nasal cavities will start to dry, crack and bleed. The stomach
will get dry and shrink, causing vomiting and heaving,” Ford said.
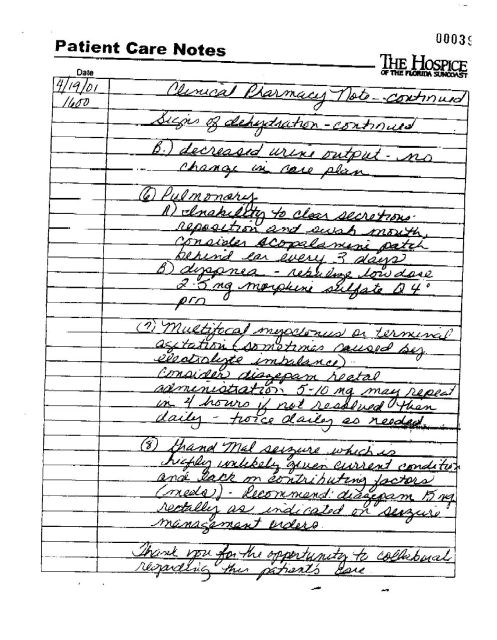
• Pulmonary
(a) Inability to clear secretions — reposition and swab mouth, consider
scopolamine patch behind ear every 3 days.
“When you first go into
dehydration, your body will automatically compensate by making saliva. But
when she gets into the stage where the stomach shrinks and nausea begins,
they’re going to stick a patch behind her ear for the nausea. What the
patch also does is dehydrate you by taking away this fluid.”
(b) Dyspnea — nebulize low dose 2-5 mg. Morphine sulfate
Q4 prn [four times a day as needed].
“Dyspnea is when you have
difficulty breathing. What they’re going to do is use a nebulizer the
way you might use for asthmatics — only instead of giving a histamine
to help her breathe, they’re going to give Terri morphine sulfate, which
only suppresses respiration more. In the later phases she’ll start gasping
for air.”
In seven to nine days, as most of her body fluids are
lost, her blood pressure will go down and her heart rate will rise. The blood
will be shunted to the central part of the body from the periphery of the
body, so that usually two to three days prior to death, the hands and feet
become extremely cold. They become mottled and have a bluish appearance.
The eyes will become so dry the patient can’t move them anymore because
there will be fluid in them.
• Multifocal myoclonus
or terminal agitation [sometimes caused by electrolyte imbalance]. Consider
diazepam rectal administration 5-10 mg. May repeat in 4 hours if not resolved
then daily — twice daily as needed.
Multifocal myoclonus means
seizures taking place in various parts of the body. “Because of the
electrolyte imbalance, Terri will begin to have seizures,” Ford said.
“She’ll start to twitch. You don’t see this in an oncology
patient because they’re already dehydrated. Even the elderly, who are
going into the natural process of death, their bodies are doing what God
created them to do — slow down.
“Our job as health-care professionals at this point
is to understand the death process and to oblige the process God has given
these people to help them in comfort measures — palliative care —
not to enhance death. But Terri’s not terminal,” Ford said. “What
they’re doing here is starving a healthy person to death. This is the
only reason why she’ll go into multifocal myoclonus.”
• Grand Mal seizure, which is highly unlikely given current
conditions and lack of contributing factors (meds) [medication]. Recommend
diazepam 15 mg. rectally as indicated in seizure management
orders.
“If she happens to make
it into a grand mal seizure, they will give her 15 mg. of valium. …
The valium won’t make this easier, it will just help to bring her to
death faster, because she won’t have the ability to fight her way out
of it,” Ford said. “Her body will not be in good shape at this
point. You wouldn’t look at her and say she was comfortable. She’s
been without food and water for a long time. She’s pretty much withered,
her skin is broken down, her metabolism is broken down, her kidneys haven’t
received anything. Her body is reacting to the lack of food.”
At this point, death is imminent.
During the Oct. 2003 tube withdrawal, Ford saw Terri before
the process began.
“They started off by dressing her in wool sweaters
and long pants, then wrapped her in a wool blanket — to ‘sweat
her out’ — to make her deyhdrate faster,” Ford said. She was
horrified, especially because it was only October and it’s still hot
in Florida in October.
“This is not a painless or dignified
way to die,” Ford said. “It’s against the law to dehydrate
and starve to death a prisoner on death row. Why should we allow it to be
done to a disabled woman — or anybody?”
The cruelty Ford has seen Terri endure is “not even believable,”
she said. “In this case, Dr. Kevorkian would be more humane than what
they intend to do to Terri.”
Contact Susan Brinkmann at fiat723@aol.com or (215)
965-4615.
http://www.cst-phl.com/050113/sixth.html